The Perceptions of Pregnancy blog, like the Researchers’ Network, aims to reach beyond boundaries and borders, and to facilitate an international and interdisciplinary conversation on pregnancy and its associated bodily and emotional experiences from the medieval to the modern. Today’s post from Jesse Olszynko-Gryn continues to explore the relationship between pregnancy testing and birth defects in the 20th century. To read Part One of Jesse’s work, click here.
In 1982, a special report in The American Journal of Nursing warned that information on the safety of ‘drugs for two in pregnancy’ was ‘scanty, hard to find and often not up to date.’ The Physicians’ Desk Reference was ‘stuffed full of the unhelpful disclaimer “the safety of drug X in human pregnancy has not been established.”’ The placenta was not a ‘barrier’, but a ‘sieve’, so only ‘medically indicated’ and ‘relatively safe’ drugs ought to be given to pregnant women. ‘No sex hormone’, it seemed, was considered ‘safe during pregnancy’; all should be avoided.[1]
Then, as now, concerns around sex hormones and birth defects focused primarily on the systemic use of synthetic estrogens and progestogens in oral contraception and the prevention of miscarriage. The previously widespread use of oral pregnancy tests, a third major source of concern, had, in 1982, recently ceased in most ‘developed’ countries.
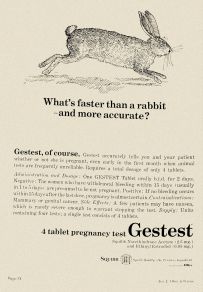
My last post explored the German origins of Gestest, the oral pregnancy test marketed in the United States by the pharmaceutical company Squibb and subject to litigation in Cheyenne, Wyoming. Here I examine the 1975 ruling by the US Food and Drug Administration (FDA) that banned Gestest and related products. I also explore the unresolved controversy over sex hormones and birth defects, which heated up again in the early 1980s.
Needless exposures
 Beginning in 1967, several research teams in Britain, Canada and the United States independently warned that the use of sex hormones in early pregnancy might cause birth defects and so presented a ‘potential public-health hazard’. Epidemiologists debated the risk-benefit ratios of oral contraception and hormone therapy, but generally agreed that it would be ‘prudent to discontinue’ the use of oral pregnancy tests ‘because acceptable alternatives are available.’[2] Even researchers who found ‘no definite evidence’ of fetal harm, still questioned the ‘safety of the tests in the absence of appropriate studies’, and cautioned physicians to ‘be careful in the use of the agents.’[3]
Beginning in 1967, several research teams in Britain, Canada and the United States independently warned that the use of sex hormones in early pregnancy might cause birth defects and so presented a ‘potential public-health hazard’. Epidemiologists debated the risk-benefit ratios of oral contraception and hormone therapy, but generally agreed that it would be ‘prudent to discontinue’ the use of oral pregnancy tests ‘because acceptable alternatives are available.’[2] Even researchers who found ‘no definite evidence’ of fetal harm, still questioned the ‘safety of the tests in the absence of appropriate studies’, and cautioned physicians to ‘be careful in the use of the agents.’[3]
This flurry of studies published in leading medical journals prompted the FDA to review the clinical evidence and to report in the Federal Register, in 1973, that the ‘diagnostic benefits’ of Squibb’s Gestest did ‘not outweigh the potential dangers from the drug in the presence of pregnancy.’ The report further noted the ‘availability of a number of very accurate chemical tests to detect pregnancy,’ and that ‘proof of the drug’s safety’ was ‘lacking.’[4]
Squibb promptly withdrew Gestest and, in March 1975, the FDA issued a decisive warning that sex hormones ‘may seriously damage the fetus’ and so ‘should not be used in early pregnancy for any purpose.’ This ‘potential risk’ also precluded the ‘use of those hormones as a diagnostic test for pregnancy. Other satisfactory tests are available.’[5] Researchers, though still undecided about oral contraception and hormone therapy, concurred that oral pregnancy tests represented ‘needless exposures’ and that their continued use was ‘not justified’.[6]
Producing doubt
The controversy over oral pregnancy tests found some closure in the United States with the FDA ban and, a few years later, with the massive settlement Squibb paid to parents of a severely malformed child whose mother had taken Gestest while pregnant. Yet researchers continued to debate the relationship between sex hormones and birth defects. In 1981, for instance, a major review of the literature concluded ‘that the use of exogenous hormones during human pregnancy has not been proved to cause developmental abnormality in nongenital organs and tissues.’[7]
The review provoked James and Audrey Nora, the husband-and-wife team of medical researchers from Denver, Colorado, who had testified against Squibb in the Wyoming trial. Their response, co-authored with a third colleague, Paul Wexler, provides crucial insights into the issues as the focus of debate shifted from statistical correlations to causal mechanisms.
They contrasted standard epidemiological methods, which sufficed to ‘unmask high-level teratogens,’ with the ‘more rigorous’ techniques needed to detect ‘low-level teratogens, which may cause birth defects in 1% or 2% of pregnancies exposed at a vulnerable period of embryogenesis’. Thalidomide and rubella, they argued, were the exceptions that proved the rule. In almost every other case, the evidence was equivocal and physicians were left ‘standing in the middle’: ‘Even with thalidomide (50% to 80% malformation rate), it took four years from the time the drug came on the market until a sufficiently compelling data base was produced to encourage its withdrawal. How much greater is the challenge to discover low-level teratogens!’
The tobacco industry, they reminded readers in 1982, continued to fund ‘epidemiologic studies refuting a causal relationship between tobacco, cancer, heart disease, and other problems.’ Was the pharmaceutical industry in the same business of producing doubt about ‘hormone-related birth defects’?[8]
Historians have already revealed how industry scientists sowed uncertainty around a range of issues from tobacco smoke to global warming.[9] Schering Chemicals, the British subsidiary of the German pharmaceutical company that marketed hormone products around the world and had perhaps the most to lose from litigation, did the same kind of thing. It openly supported research casting doubt on the relationship between not only sex hormones and birth defects, but also oral contraceptives and potentially fatal blood clots in young, otherwise healthy women.[10]
Today no one would dispute that contraceptive pills increase a woman’s risk of developing a blood clot.[11] The jury is still out on birth defects.[12] With a UK government inquiry underway and an abundance of unused corporate and state archives on hand, the time is ripe for historians to dig deeper into this unresolved controversy.
Jesse Olszynko-Gryn is a Wellcome Trust Research Fellow in the Department of History and Philosophy of Science and Director of Studies at St John’s College, University of Cambridge. He is currently writing a book on the history of pregnancy testing in Britain, from around 1900 to the present. He is also organising a conference on the contested history of hormone pregnancy tests. For more information, click here.
Image: This whimsical advertisement for Squibb’s Gestest, intended not for women, but for their doctors, took aim at ‘the rabbit test’, the standard medical method of ascertaining pregnancy in the United States at the time that also gave rise to the American euphemism, ‘The rabbit died’. American Journal of Obstetrics and Gynecology, 15 Apr. 1965, p. 74.
[1] Sally Wicklund, ‘Special report: Drugs for two in pregnancy’, The American Journal of Nursing, 82, Jun. 1982, pp. 980-981.
[2] Dwight T. Janerich, Joyce M. Piper and Donna M. Glebatis, ‘Oral contraceptives and congenital limb-reduction defects’, The New England Journal of Medicine, 291, 3 Oct. 1974, pp. 697-700.
[3] Godfrey P. Oakley, Jr., J. William Flynt, Jr. and Arthur Falek, ‘Hormonal pregnancy tests and congenital malformations’, The Lancet, 2, 4 Aug. 1973, pp. 256-257.
[4] Federal Register, 38, 7 February 1973, p. 3534.
[5] ‘Warning on use of sex hormones in pregnancy’, FDA Drug Bulletin, 5, Jan.-Mar. 1975, p. 4.
[6] Dwight T. Janerich, J. Marin Dugan, Susan J. Standfast and Linda Strite, ‘Congenital heart disease and prenatal exposure to exogenous sex hormones’, British Medical Journal, 1, 23 Apr. 1977, pp. 1058-1060.
[7] James G. Wilson and Robert L. Brent, ‘Are female sex hormones teratogenic?’ American Journal of Obstetrics and Gynecology, 141, 1 Nov. 1981, pp. 567-580, on p. 577.
[8] James J. Nora, Audrey H. Nora and Paul Wexler, ‘Exogenous sex hormones and birth defects: Continuing the dialogue’, American Journal of Obstetrics and Gynecology, 144, 1 Dec. 1982, pp. 860-862.
[9] Robert N. Proctor, Cancer Wars: How Politics Shapes What We Know and Don’t Know about Cancer (New York: Basic Books, 1995); Naomi Oreskes and Erik M. Conway, Merchants of Doubt: How a Handful of Scientists Obscured the Truth on Issues from Tobacco Smoke to Global Warming (New York: Bloomsbury Press, 2010).
[10] Richard A. Wiseman and Kenneth D. MacRae, ‘Oral contraceptives and the decline in mortality from circulatory disease’, Fertility and Sterility, 35, Mar. 1981, pp. 277-283; R.A. Wiseman and I.C. Dodds-Smith, ‘Cardiovascular birth defects and antenatal exposure to female sex hormones: A reevaluation of some basic data’, Teratology, 30, Dec. 1984, pp. 359-370.
[11] Yana Vinogradova, Carol Coupland and Julia Hippisley-Cox, ‘Use of combined oral contraceptives and risk of venous thromboembolism: Nested case-control studies using the QResearch and CPRD databases’, The BMJ, 2015;350:h2135, doi: 10.1136/bmj.h2135 (published online 26 May 2016).
[12] Brittany M. Charlton, Ditte Mølgaard-Nielsen, Henrik Svanström, Jan Wohlfahrt, Björn Pasternak and Mads Melbye, ‘Maternal use of oral contraceptives and risk of birth defects in Denmark: Prospective, nationwide cohort study’, BMJ 2016;352:h6712, doi: 10.1136/bmj.h6712 (Published 6 Jan. 2016).
Pingback: Whewell’s Gazette: Year 03, Vol. #18 | Whewell's Ghost